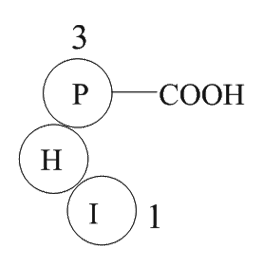
Angiotensin 1/2 (5-7) (Synonyms: H2N-Ile-His-Pro-OH ) |
| Catalog No.GP10079 |
Products are for research use only. Not for human use. We do not sell to patients.
Sample solution is provided at 25 µL, 10mM.
GlpBio Products Cited In Reputable Papers
Product Documents
Quality Control & SDS
- View current batch:
- Purity: >98.00%
- COA (Certificate Of Analysis)
- SDS (Safety Data Sheet)
- Datasheet
| Cas No. | SDF | ||
| Synonyms | H2N-Ile-His-Pro-OH | ||
| Canonical SMILES | N[C@@H]([C@H](C)CC)C(N[C@@H](CC1=CNC=N1)C(N2CCC[C@@H]2C(O)=O)=O)=O | ||
| Formula | C17H27N5O4 | M.Wt | 365.43 |
| Solubility | ≥36.5mg/mL in DMSO | Storage | Store at -20°C |
| General tips | Please select the appropriate solvent to prepare the stock solution according to the
solubility of the product in different solvents; once the solution is prepared, please store it in
separate packages to avoid product failure caused by repeated freezing and thawing.Storage method
and period of the stock solution: When stored at -80°C, please use it within 6 months; when stored
at -20°C, please use it within 1 month. To increase solubility, heat the tube to 37°C and then oscillate in an ultrasonic bath for some time. |
||
| Shipping Condition | Evaluation sample solution: shipped with blue ice. All other sizes available: with RT, or with Blue Ice upon request. | ||
Complete Stock Solution Preparation Table
| Prepare stock solution | |||
|
1 mg | 5 mg | 10 mg |
| 1 mM | 2.7365 mL | 13.6825 mL | 27.365 mL |
| 5 mM | 0.5473 mL | 2.7365 mL | 5.473 mL |
| 10 mM | 0.2737 mL | 1.3683 mL | 2.7365 mL |
In vivo Formulation Calculator (Clear solution)
Step 1: Enter information below (Recommended: An additional animal making an allowance for loss during the experiment)
 g
g
 μL
μL

Step 2: Enter the in vivo formulation (This is only the calculator, not formulation. Please contact us first if there is no in vivo formulation at the solubility Section.)
Calculation results:
Working concentration: mg/ml;
Method for preparing DMSO master liquid: mg drug pre-dissolved in μL DMSO ( Master liquid concentration mg/mL, Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug. )
Method for preparing in vivo formulation: Take μL DMSO master liquid, next addμL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O, mix and clarify.
Method for preparing in vivo formulation: Take μL DMSO master liquid, next add μL Corn oil, mix and clarify.
Note: 1. Please make sure the liquid is clear before adding the next solvent.
2. Be sure to add the solvent(s) in order. You must ensure that the solution obtained, in the previous addition, is a clear solution before proceeding to add the next solvent. Physical methods such as vortex, ultrasound or hot water bath can be used to aid dissolving.
3. All of the above co-solvents are available for purchase on the GlpBio website.
Related Products
- GP10100 immunoglobulin light chain variable region fragment [Homo sapiens]
- GP10078 Papain Inhibitor
- GP10099 amyloid A protein fragment [Homo sapiens]
- GP10031 Leptin (116-130) amide (mouse)
- GP10072 Pro-Adrenomedullin (153-185), human
- GP10069 Parathyroid hormone (1-34) (human)
- GP10115 GTP-Binding Protein Fragment, G alpha
- GP10124 Anti-Inflammatory Peptide 1
- GP10132 erbB-2
- GP10109 Adrenorphin
- GP10028 tumor protein p53 binding protein fragment [Homo sapiens]/[Mus musculus]
- GP10074 Angiotensin 1/2 (1-5)
- GP10051 Beta-Lipotropin (1-10), porcine
- GP10001 vitamin D binding protein precursor (353-363) [Homo sapiens]
- GP10101 Beta-Sheet Breaker Peptide iAβ5
- GP10106 Parathyroid Hormone (1-34), bovine
- GP10016 Lamin fragment
Reviews
Average Rating: 5 ★★★★★ (Based on Reviews and 30 reference(s) in Google Scholar.)
GLPBIO products are for RESEARCH USE ONLY. Please make sure your review or question is research based.
Required fields are marked with *