Dencichin (Dencichine) |
| Catalog No.GC31230 |
Dencichin is a non-protein amino acid originally extracted from Panax notoginseng, and can inhibit HIF-prolyl hydroxylase-2 (PHD-2) activity.
Products are for research use only. Not for human use. We do not sell to patients.
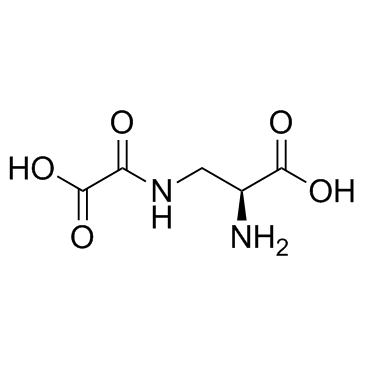
Cas No.: 5302-45-4
Sample solution is provided at 25 µL, 10mM.
Dencichin is a non-protein amino acid originally extracted from Panax notoginseng, and can inhibit HIF-prolyl hydroxylase-2 (PHD-2) activity.
Dencichin (β-ODAP, 10 μM, 50 μM, 100 μM and 200 μM) increases HRE expression by 1.3±0.09, 2.5±0.07, 4.2±0.15 and 1.3±0.07 fold respectively compared to control. Dencichin has intermolecular interactions with PHD-2[1]. Dencichin (10 μM, 100 μM, 1 mM) significantly inhibits cell proliferation and extracellular matrix (ECM) proteins accumulation of HBZY-1 cells, and reduces the secretion of collagen I (Col I), collagen IV (Col IV), and fibronectin (FN)[2].
Dencichin improves metabolism disorder in diabetic nephropathy (DN) secondary to type II diabetes mellitus (DM) model. Dencichin (80, 160 mg/kg/day, p.o.) significantly prevents the up-regulation of TCH, TG, LDL, and HbAlc and the down-regulation of HDL in DN rats induced by STZ injection. Dencichin also attenuates renal injury induced in the DN secondary to type II DM model. Dencichin alleviates pancreas damage in the STZ-induced DN model. Dencichin regulates protein expression in the TGF-β/Smad signalling pathway in STZ-induced DN models[2].
[1]. Eslavath RK, et al. β-N-oxalyl-L-α, β- diaminopropionic acid induces HRE expression by inhibiting HIF-prolyl hydroxylase-2 in normoxic conditions. Eur J Pharmacol. 2016 Nov 15;791:405-411. [2]. Jie L, et al. Dencichine ameliorates kidney injury in induced type II diabetic nephropathy via the TGF-β/Smad signalling pathway. Eur J Pharmacol. 2017 Oct 5;812:196-205.
Average Rating: 5 (Based on Reviews and 40 reference(s) in Google Scholar.)
GLPBIO products are for RESEARCH USE ONLY. Please make sure your review or question is research based.
Required fields are marked with *