ANGIOTENSIN Ⅱ
Angiotensin Ⅱ human, Ang Ⅱ, are the other names of the Angiotensin Ⅱ. Chemically, it belongs to the family having ligands and named as Angiotensin. It is a synthetic and acts as a vasoconstrictor.
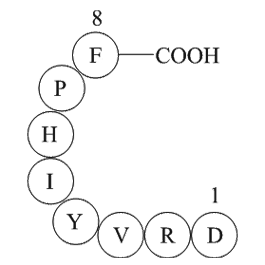
Angiotensin Ⅱ is a small peptide consisting of a sequence of just eight amino acid residues; thus, it is more appropriately termed as an octapeptide. Its primary structure is Asp-Arg-Val-Tyr-Ile-His-Pro-Phe which is also present in Figure 2 . It is also naturally produced in the body and performs several physiological functions in the body, thus more appropriately regarded as a hormone.
Physiology
Angiotensin Ⅱ(GP10023) is naturally and locally produced in the human body mainly in the brain, heart, vasculature adrenals and kidneys tissues, through several pathways which are presented in Figure 1 and, specifically through renin-angiotensin system (RAS) is shown along with the peptides sequences in Figure 2 . This locally produced Angiotensin Ⅱ mainly cause the vascular inflammatory responses. In the pulmonary circulation (blood circulating through the lungs), angiotensinogen (originally produced in the liver) is biochemically converted into Angiotensin Ⅰ which is an inactive form by the activity of Renin that is itself produced by the kidney cells in the juxtaglomerular region. Angiotensin Ⅰ is also a small peptide consisting of just ten amino acid residues. In the last step, Angiotensin-Converting Enzyme (ACE) finally converts Angiotensin Ⅰ into Angiotensin Ⅱ. This pathway is ACE-dependent; there is also a way that is ACE-dependent. In this pathway, different enzymes produce Angiotensin Ⅱ either from Angiotensinogen (i.e., tissue plasminogen activator (t-PA), Cathepsin G and Tonin) or Angiotensin Ⅰ (i.e., chymostatin-sensitive Ang II-generating enzyme (CAGE), Cathepsin G and Chymase).
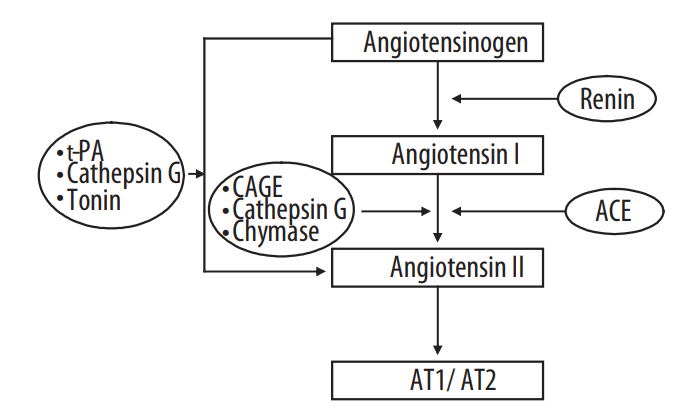
Figure 1 Biosynthesis of Angiotensin Ⅱ through ACE-dependent and ACE-independent pathways
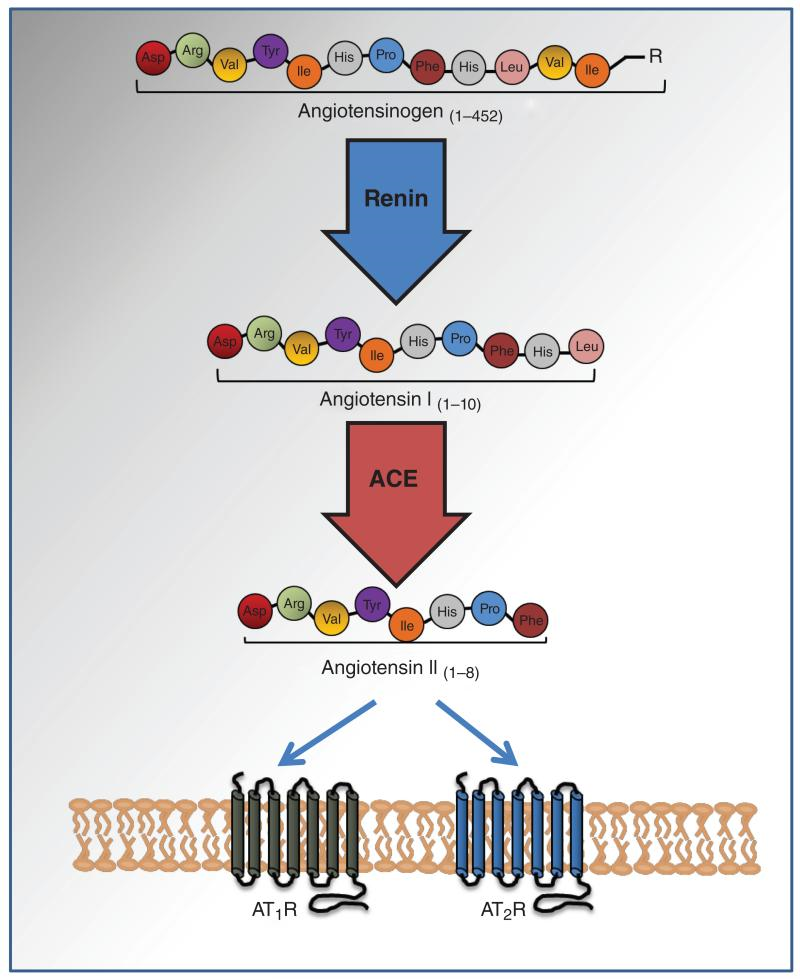
Figure 2 Biosynthesis of Angiotensin Ⅱ. The primary structure of the Angiotensin Ⅱ is also shown.
In a clinical research study, Angiotensin Ⅱ is proposed as a therapeutic candidate for the treatment of Distributive shock that is also known as vasodilatory shock or simply shock; especially when it has become refractory to the traditional drug like catecholamines and arginine vasopressin. In this pathological condition, there is a vasodilation (a condition in which the blood vessels relax) especially in the peripheral blood vessels; and the systemic blood pressure is critically reduced and thereof the blood supply to the vital organs becomes limited. This condition is common in the critically ill patients. The clinically relevant parameters, the Blood Pressure and the Survival Rate has experimentally been shown to improve as evident from the graphs in Figure 3 and Figure 4, respectively.
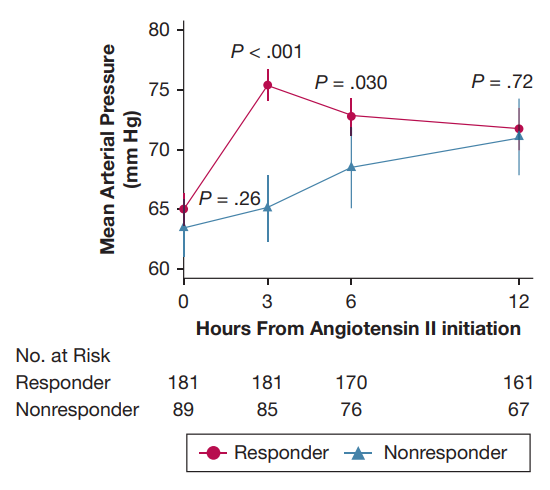
Figure 3 The Hemodynamic response, i.e., rise in the Blood Pressure level, to the Angiotensin Ⅱ intravenous infusion. The Blood Pressure level was restored to the normal within three hours of the Angiotensin Ⅱ intravenous infusion
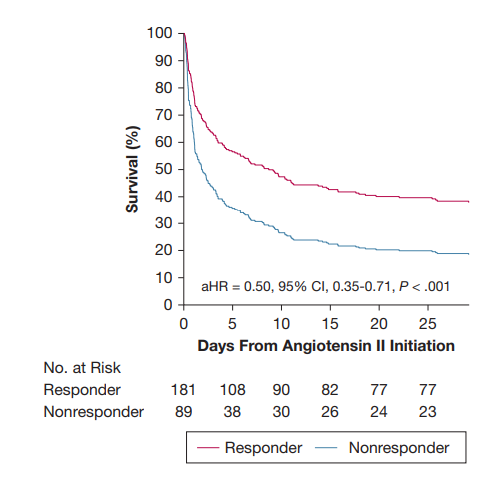
Figure 4 The Survival Rate in the Shock patient is improved after the Angiotensin Ⅱ intravenous infusion
Allergic Asthma is a respiratory disease that is marked by prolonged inflammation. In this pathological condition, group 2 innate lymphoid cells (ILC2s) of the lung epithelium are very important as they express Angiotensin Ⅱ Type 1 receptor (AT1) which is the legitimate receptor for the Angiotensin Ⅱ ligand along with the receptors for a wide spectrum of the ligand molecules like cytokines, lipid mediators, neurotransmitters, hormones, and nutrients. Group 2 innate lymphoid cells (ILC2s) play a number of regulatory roles, that means that they either leads to the homeostasis or the inflammatory responses depending upon the nature and concentration of the ligand. Moreover, upon the exposure to the allergen, the Angiotensin Ⅱ octapeptide is upregulated via the renin-angiotensin system (RAS) in these cells, i.e., group 2 innate lymphoid cells (ILC2s) and thereby these are activated.
After the allergen exposure like Papain all the major components of the renin-angiotensin system (RAS) including the precursors like AGT and enzymes like Renin and ACE, are upregulated and resultantly the final product, i.e., Angiotensin Ⅱ also get upregulated in the epithelial cells (CD45−EpCAM+) from lungs. This observation is graphically represented in Figure 5.
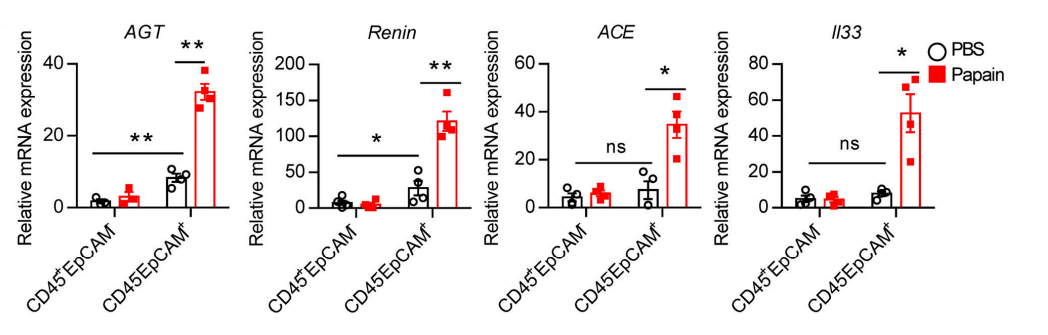
Figure 5 The mRNA expression of all the major players in the renin-angiotensin system (RAS) including AGT, Renin and ACE along with the experimental control of II33. It was measured in two different cell lines, i.e., the lymphocytes (CD45+EpCAM−) and epithelial cells (CD45−EpCAM+) from lungs.
This observation suggests that inhibition of Angiotensin Ⅱ could be a valid option for the treatment of inflammation in asthma.
Angiotensin Ⅱ causes vascular inflammation, i.e., inflammation of the blood vessels, when its molecules interact and bind to its respective receptor protein that are present on the surface of the cell. For Angiotensin Ⅱ, there are two distinct types of the receptors; first, Angiotensin Ⅱ Type 1 receptor (AT1) while the other is the Angiotensin Ⅱ Type Ⅱ (AT2). Both these receptors are the 7 trans-membrane receptors, i.e., they both individually have seven helices forming a domain that is embedded in the hydrophobic core of the lipid bilayer in the plasma membrane of the cell. Out of these two types, Angiotensin Ⅱ Type 1 receptor (AT1) is expressed by the smooth muscle cells of the vasculature specifically called as vascular smooth muscle cells (VSMCs); and interestingly most of the effects on the cardiovascular system, for example vascular inflammation, are mediated by the Angiotensin Ⅱ- Angiotensin Ⅱ Type 1 receptor (AT1) interaction. There are three distinct phases of the inflammation process namely increment in the vascular permeability (via the endothelial injury), leukocyte infiltration (it happens as leukocytes leave the blood circulation and enter the perivascular space. This infilteration process has three distinct phases namely rolling, adhesion and transmigration. and tissue remodelling. Angiotensin Ⅱ specifically promotes adhesion of the leukocytes mainly monocytes and neutrophils to the endothelial layer of artery wall) and tissue remodeling (the proliferation of the VSMCs is increased via autocrine and paracrine growth factor namely basic fibroblast growth factors (bFGF) having mitogenic effect, platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and transforming growth factor-b (TGF-b)). It has been scientifically proven that the Angiotensin Ⅱ increases each of the phases of inflammation process which is a common landmark of a number of vascular diseases and other diseases as well like. To name a few diseases, myocardial infarction, stroke, atherosclerosis, endothelial dysfunction, renal failure, hypertension and diabetes. This is represented in Figure 6 and Figure 7.
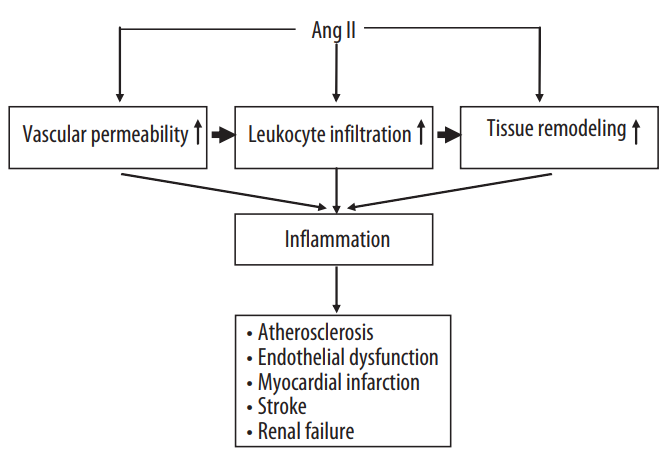
Figure 6 Angiotensin Ⅱ promotes the overall inflammation process particularly at each phase
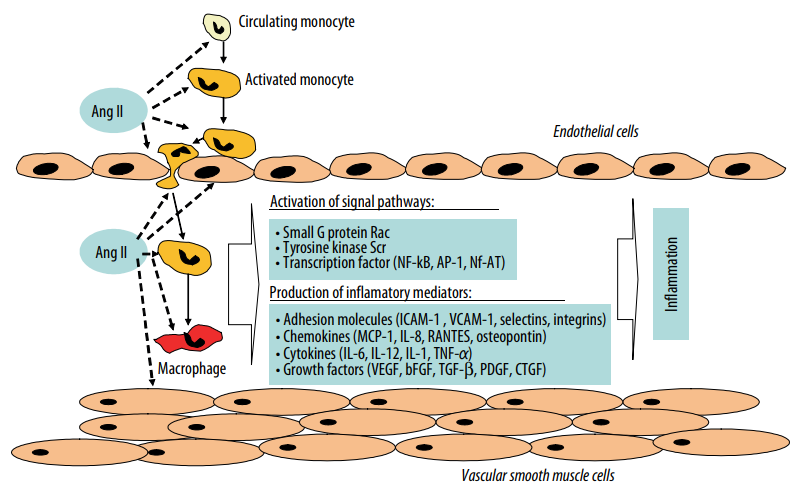
Figure 7 Angiotensin Ⅱ promotes inflammation process via increasing the vascular permeability, adhesion of the leukocytes (monocytes and neutrophils) with the endothelial layer of the arterial wall and their transmigration, proliferation and fibrosis in the Vascular Smooth Muscle Cells (VSMCs) leading to the tissue remodelling.
Besides acting as a growth factor, regulating the cellular growth and fibrosis, i.e., formation of the connective tissue, and as a proinflammatory as it promotes inflammatory processes. Angiotensin Ⅱ also induces the production of the Reactive Oxygen Species (ROS) specifically in the endothelium, adventitia, VSMCs and fibroblasts. This effect is also mediated by the Angiotensin Ⅱ- Angiotensin Ⅱ Type 1 receptor (AT1) interaction.













Comments