The Most Painful Trigeminal Meuralgia in Humans
Therapeutic Target is coming
Trigeminal neuralgia is the most common cranial nerve disease, characterized by recurrent paroxysmal severe pain in the distribution area of the trigeminal nerve on one side of the face. The patient's daily activities, such as eating, drinking, talking, washing face, brushing teeth, etc., can cause severe pain, and some patients can even cause excruciating pain when the breeze blows. Therefore, trigeminal neuralgia is also known as "the first pain in the world", and some patients even choose to commit suicide to end the pain. Those who endure pain also tend to have lower quality of life, anxiety and depression.
The pathophysiological molecular mechanisms of trigeminal neuralgia still remain poorly understood so far, leading to a severe lack of therapeutic drugs. There is currently only one drug approved by the FDA for the treatment of trigeminal neuralgia, Carbamazepine, which is mainly used to control seizures and can broadly and non-specifically inhibit neural activity, but its side effects are also very obvious. In addition, some patients choose surgery. But long-term follow-up shows that, even with maximum medical and surgical treatment, many people with trigeminal neuralgia experience pain recurrences.
On August 3, 2022, researchers at Johns Hopkins University published a research paper titled: Identification of the NRF2 transcriptional network as a therapeutic target for trigeminal neuropathic pain in Science Advances, a sub-journal of Science.
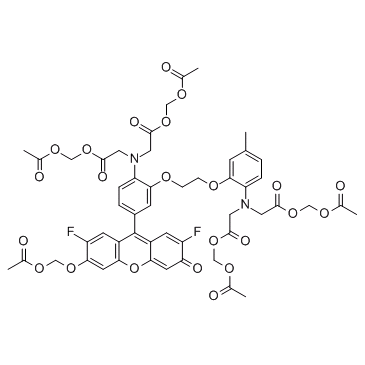
This study shows that reactive oxygen species (ROS) accumulate in the cerebrospinal fluid of patients with trigeminal neuralgia, and they directly activate the pain ion channel TRPA1, which further identifies the NRF2 transcriptional network as a potential therapeutic target for trigeminal neuralgia. Activation of the NRF2 antioxidant transcriptional network has the same analgesic effect as inhibition of TRPA1.
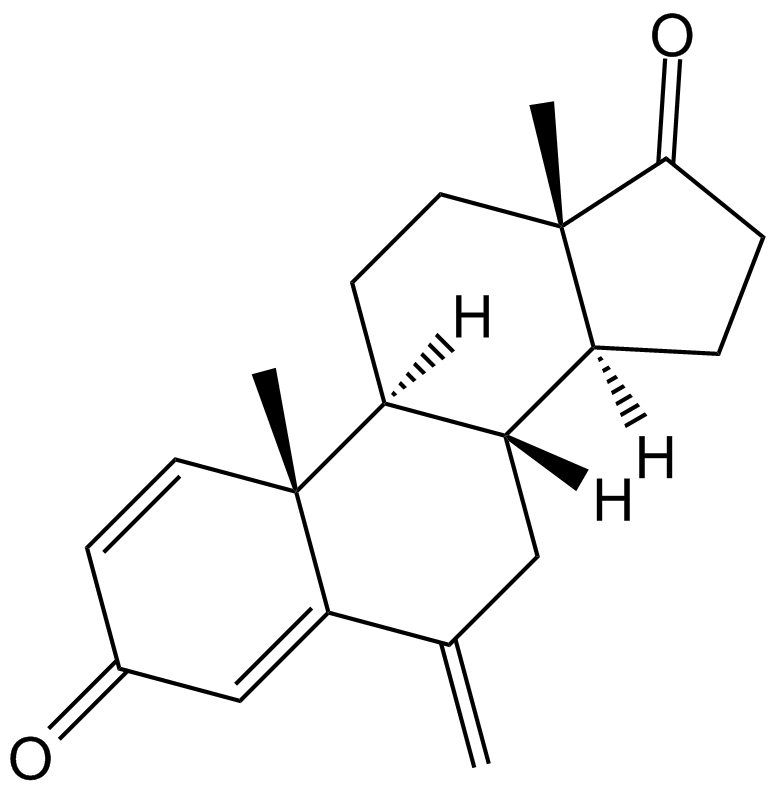
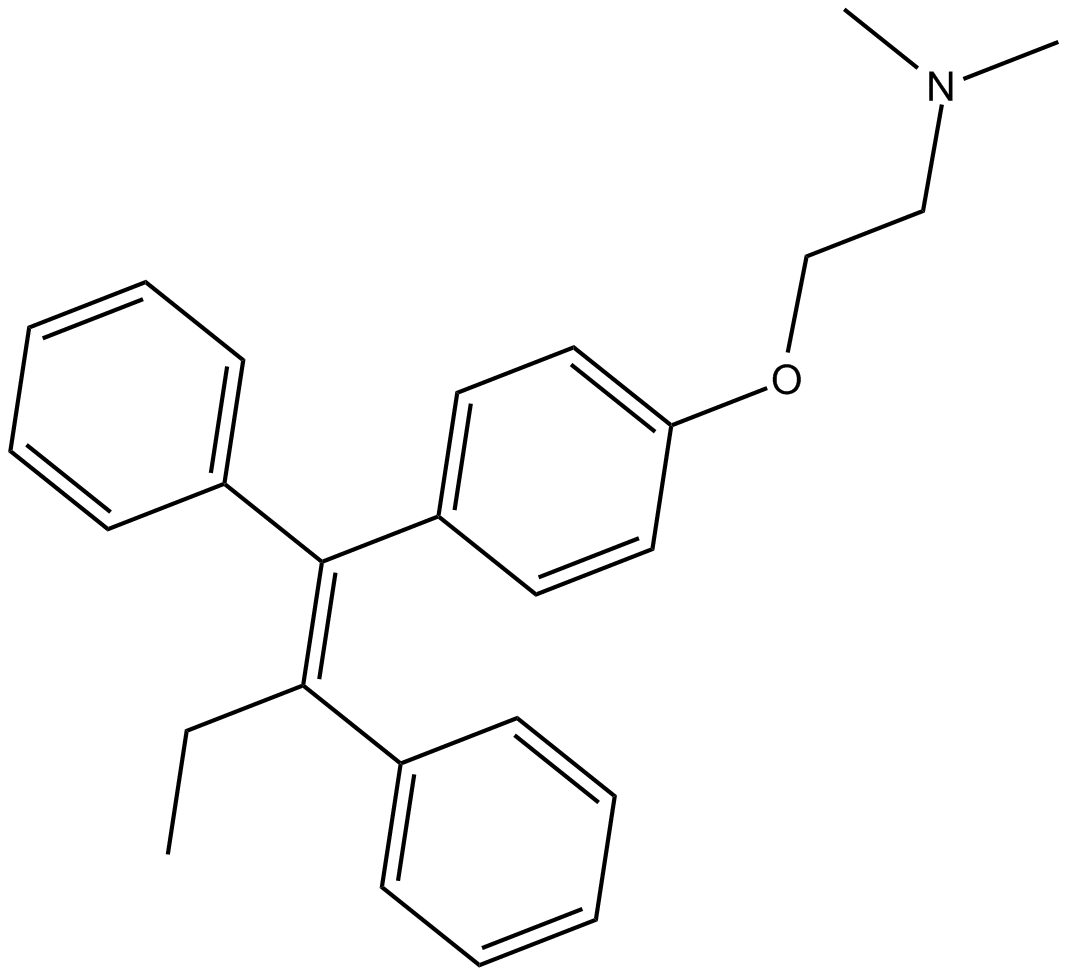
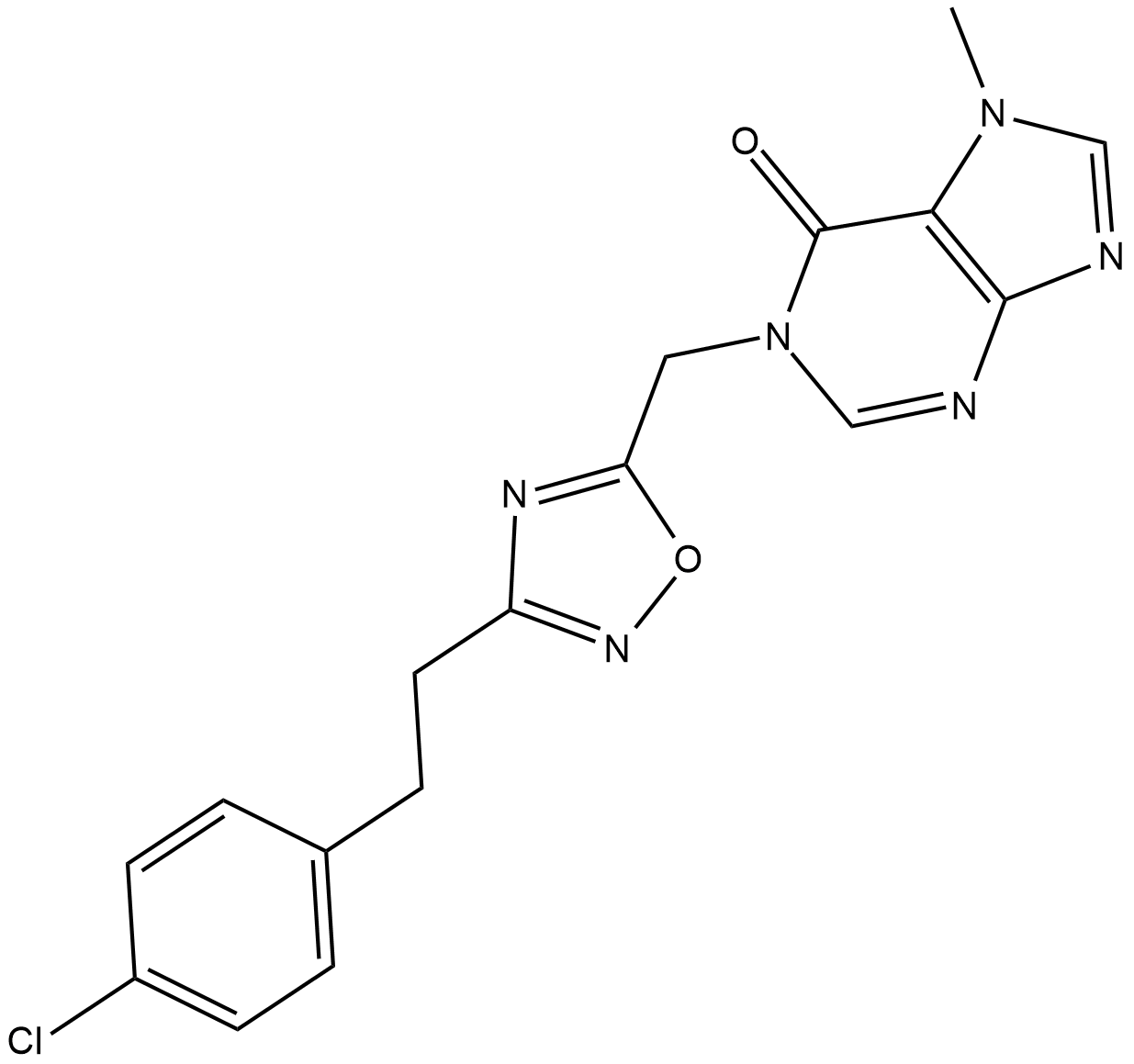
Using a transcriptome-guided drug discovery strategy, this study identifies two NRF2 network regulators as potential therapeutics. One of the drug candidates, Exemestane, is FDA-approved for breast cancer, so it could be a promising alternative for treating trigeminal neuralgia.
In this latest study, the research team found evidence that increased oxidative stress contributes to trigeminal neuropathic pain. Like human patients, mouse models of trigeminal neuralgia also accumulate reactive oxygen species (ROS), some of which directly activate the pain ion channel TRPA1.
The research team further found that inhibiting TRPA1 pharmacologically or at the genetic level reduced pain. However, attempts to directly inhibit TRPA1 have been difficult to translate clinically, and previous studies have all failed.
In this study, the research team found that activating the NRF2 antioxidant transcriptional network had as potent analgesic effects as direct inhibition of TRPA1, while also reversing underlying oxidative stress.
Using a transcriptome-guided drug discovery strategy, the research team identified two NRF2 network regulators, Exemestane and JQ-1. Exemestane has been approved by the FDA for the treatment of estrogen receptor-positive breast cancer. Therefore, the drug can be easily repurposed for research in the treatment of trigeminal neuralgia and may be a promising alternative therapy for the treatment of trigeminal neuralgia.
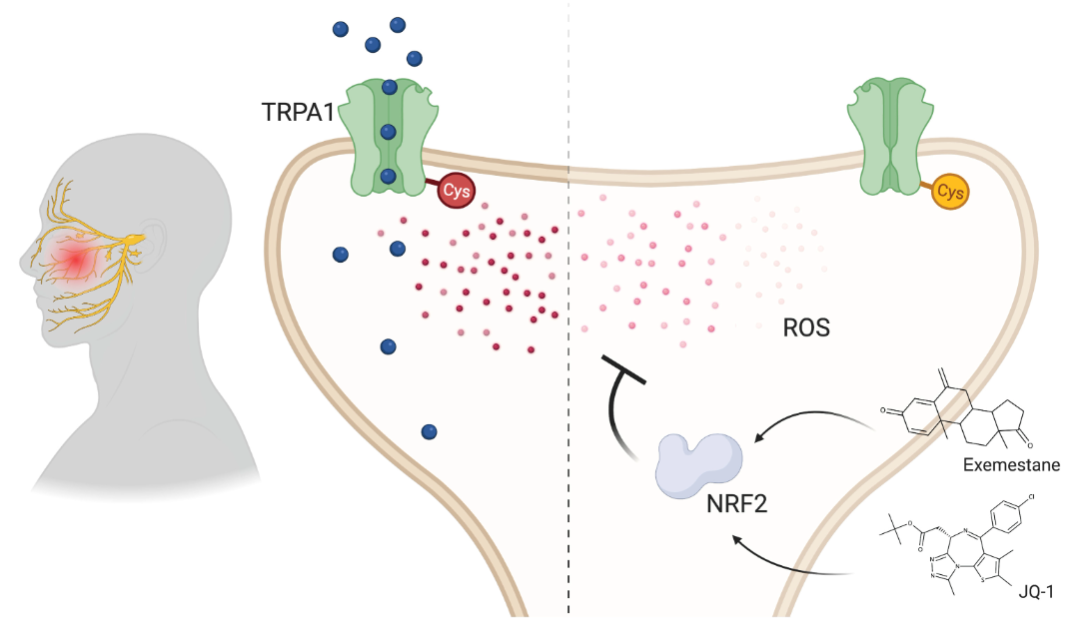
Overall, this study uses a combination of clinical, molecular and computational approaches to identify the NRF2 transcriptional network as a potential therapeutic target for trigeminal neuralgia. Using a transcriptome-guided drug discovery approach, Exemestane and JQ-1 were identified as two candidate NRF2 network modulators for the treatment of trigeminal neuralgia. Activating the NRF2 transcriptional network may be a therapeutic approach to ameliorate pain through redox control compared to current drugs that reduce pain by inhibiting nerve firing.
Paper link:
https://www.science.org/doi/10.1126/sciadv.abo5633














Comments