Oxaliplatin (Synonyms: Lipoxal, NSC 266046, RP 54780) |
| Catalog No.GC17716 |
Oxaliplatin is a cytotoxic chemotherapy drug used to treat cancer.
Products are for research use only. Not for human use. We do not sell to patients.
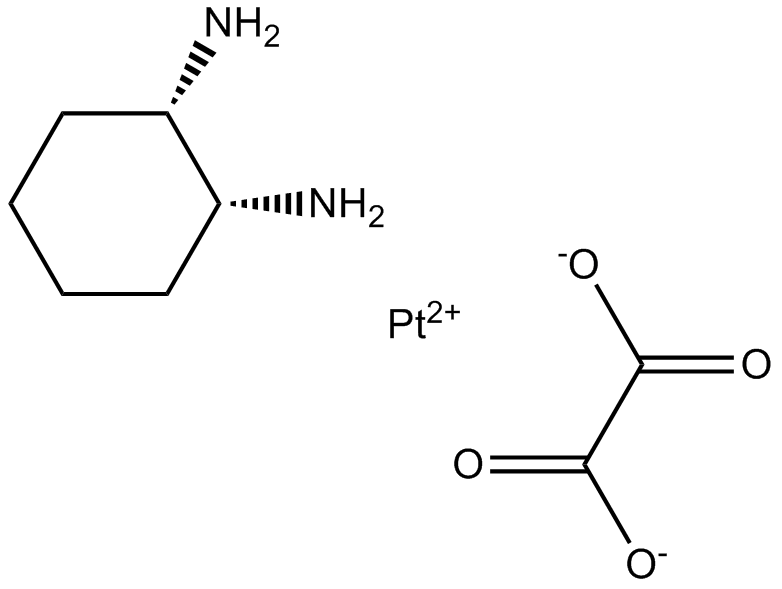
Cas No.: 61825-94-3
Sample solution is provided at 25 µL, 10mM.
Oxaliplatin is a cytotoxic chemotherapy drug used to treat cancer. Oxaliplatin works by interfering with the development of DNA in a cell. This helps to treat cancer which is caused by cells rapidly growing and dividing out of control.
Oxaliplatin can induce DNA damage in cancer cells. Besides,oxaliplatin can interfere with the cell cycle, promote apoptosis, and induce autophagy in tumor cells[2,3]. Oxaliplatin inhibited cell viability, migration, and cloning formation of OSCC cells and induced cell death in vitro[1]. Oxaliplatin inhibited the growth of HCCLM3 and Hep3B cells.Downregulation of the anti-apoptotic proteins Bcl-2 and Bcl-xL and upregulation of the pro-apoptotic protein Bax during oxaliplatin-induced apoptosis[6]. Oxaliplatin was found to be active against C32 and G361 cell lines with IC50 values of 49.48 and 9.07 uM (1 h exposure), 9.47 and 1.30 uM (4 h exposure), and 0.98 and 0.14 uM (24 h exposure), respectively. At a 24 h exposure oxaliplatin appears to be significantly more active than cisplatin against the G361 cell line[4]. 85-88% of all platinum from oxaliplatin was bound to plasma proteins within the first 5 h with an average half-life of 1.71 +/- 0.06 h. When oxaliplatin was incubated in whole blood, the erythrocytes took up 37.1 +/- 2.1% of the total platinum in 2 h (maximum uptake) which was not exchangeable into plasma[5].
The in vivo anticancer effect of oxaliplatin was studied using a nude mouse subcutaneously implanted with CAL27 cells. The average volume of tumors was markedly smaller in the oxaliplatin group than in the control group. Therefore, these results indicated that oxaliplatin inhibited the growth of xenograft OSCC cells in vivo, which was accompanied by the upregulated expression of PARP1[1]. Oxaliplatin-treated mice displayed reduced weight gain, mechanical allodynia, and exploratory behavior deficits that were not significantly improved by exercise[7]. When investigated oxaliplatin-induced haematological toxicities and splenomegaly in mice, Blood analysis showed dose dependent decreases in white and red blood cell counts, and significant changes in haematological indices.Spleen weight was significantly increased indicating splenomegaly, and red pulp tissue exhibited substantial dysplasia[8]. Oxaliplatin-treated mice displayed reduced weight gain and behavioral deficits. Mice treated over a shorter course had significantly increased STAT3 phosphorylation in gastrocnemius muscles. Mice receiving extended oxaliplatin treatment demonstrated reduced hindlimb muscle mass with upregulation of myopathy-associated genes Foxo3, MAFbx, and Bnip3[9].
References:
[1]. Li D, Kou Y, et,al. Oxaliplatin induces the PARP1-mediated parthanatos in oral squamous cell carcinoma by increasing production of ROS. Aging (Albany NY). 2021 Jan 20;13(3):4242-4257. doi: 10.18632/aging.202386. Epub 2021 Jan 20. PMID: 33495407; PMCID: PMC7906208.
[2]. Wang X, Li M, et,al. On-Demand Autophagy Cascade Amplification Nanoparticles Precisely Enhanced Oxaliplatin-Induced Cancer Immunotherapy. Adv Mater. 2020 Aug;32(32):e2002160. doi: 10.1002/adma.202002160. Epub 2020 Jun 28. PMID: 32596861.
[3]. Yan S, Zhou N, et,al. PFKFB3 Inhibition Attenuates Oxaliplatin-Induced Autophagy and Enhances Its Cytotoxicity in Colon Cancer Cells. Int J Mol Sci. 2019 Oct 30;20(21):5415. doi: 10.3390/ijms20215415. PMID: 31671668; PMCID: PMC6862230.
[4]. Mohammed MQ, Retsas S. Oxaliplatin is active in vitro against human melanoma cell lines: comparison with cisplatin and carboplatin. Anticancer Drugs. 2000 Nov;11(10):859-63. doi: 10.1097/00001813-200011000-00010. PMID: 11142694.
[5]. Pendyala L, Creaven PJ. In vitro cytotoxicity, protein binding, red blood cell partitioning, and biotransformation of oxaliplatin. Cancer Res. 1993 Dec 15;53(24):5970-6. PMID: 8261411.
[6]. Wang Z, Zhou J, et,al. Oxaliplatin induces apoptosis in hepatocellular carcinoma cells and inhibits tumor growth. Expert Opin Investig Drugs. 2009 Nov;18(11):1595-604. doi: 10.1517/13543780903292626. PMID: 19780708.
[7]. Lees JG, Abdulla M, et,al. Effect of exercise on neuromuscular toxicity in oxaliplatin-treated mice. Muscle Nerve. 2021 Aug;64(2):225-234. doi: 10.1002/mus.27329. Epub 2021 Jun 12. PMID: 34036599.
[8]. Lees JG, White D, et,al. Oxaliplatin-induced haematological toxicity and splenomegaly in mice. PLoS One. 2020 Sep 2;15(9):e0238164. doi: 10.1371/journal.pone.0238164. PMID: 32877416; PMCID: PMC7467301.
[9]. Feather CE, Lees JG, et,al. Oxaliplatin induces muscle loss and muscle-specific molecular changes in Mice. Muscle Nerve. 2018 Apr;57(4):650-658. doi: 10.1002/mus.25966. Epub 2017 Oct 6. PMID: 28881481.
Average Rating: 5 (Based on Reviews and 28 reference(s) in Google Scholar.)
GLPBIO products are for RESEARCH USE ONLY. Please make sure your review or question is research based.
Required fields are marked with *





